When ENT Symptoms Are Driven by the Nervous System (Part 1)
Why a Normal Workup Can Still Point to a Real Diagnosis
First let me point out that ENT symptoms like sinus pressure, ear fullness, tinnitus, throat clearing, dizziness, or reflux-like sensations deserve a thorough medical evaluation.
Before considering neurologic causes, it is essential to:
Rule out infection, inflammation, tumors and structural disease
Evaluate for allergic, reflux-related, autoimmune, and metabolic contributors
Review medication side effects and environmental exposures
This step matters because some causes are treatable and time-sensitive, and missing them can delay appropriate care.
But here’s an important truth many patients encounter:
Sometimes the workup is thorough - and still comes back “normal.”
Normal imaging, scopes, hearing tests, or labs do not mean symptoms are imagined or insignificant. They often mean the issue is functional rather than structural - rooted in how the nervous system regulates blood flow, sensation, and reflexes.
When ENT testing is unrevealing but symptoms persist, neurologic mechanisms should be considered — not as a last resort, but as a logical next step.
There are three major nervous-system–driven processes that I see commonly in clinic…let’s explore them one by one.
Sinus Headaches
If you follow me on social, you know by now that 80-90% of people with sinus headaches actually meet criteria for migraine. Migraine is not just a headache disorder - it is a neurovascular inflammatory condition involving abnormal sensory processing and blood vessel signaling. Vestibular migraine was officially “named” in 2012 and I anticipate “sinus migraine” will be the next variation officially recognized.
How it works:
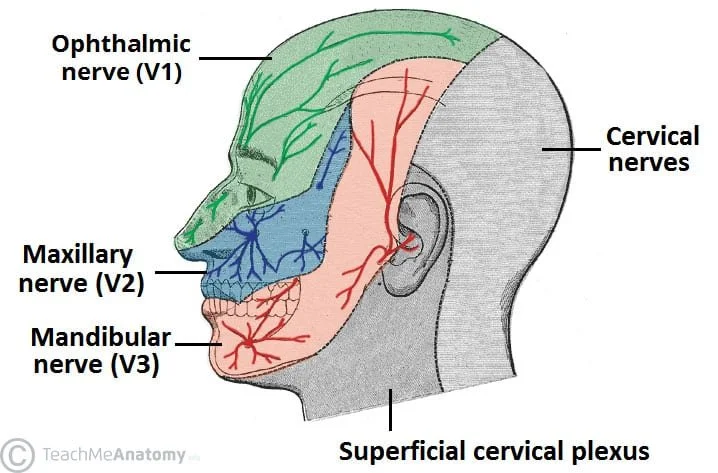
The trigeminal nerve (cranial nerve V) is the primary sensory nerve of the face, sinuses, nasal cavity, teeth, jaw, and much of the head and neck. Migraine disorders are characterized by trigeminal neurovascular inflammation.
It has three major branches:
V1 (ophthalmic) – forehead, eyes, upper nasal cavity, frontal/ethmoid sinuses
V2 (maxillary) – cheeks, upper teeth, maxillary sinuses, nasal mucosa
V3 (mandibular) – jaw, lower teeth, tongue sensation, chewing muscles/throat muscles/eardrum muscles (*this is important)
This is why so many ENT symptoms map back to trigeminal signaling. But the trigeminal nerve does far more than sensation. As noted above with * it also supplies muscles in the jaw, back of the throat and middle ear. It’s likely this nerve supply that can lead to jaw pain, ear fullness, ear popping, and tinnitus during an episode.
There is also an special branch of the nervous system called autonomic nervous system with a specific type of nerve fibers (parasympathetic) that travel with the trigeminal nerve - these nerves impact blood vessels and glands and when activated gives you the sensation of nasal congestion, runny nose, watery eyes, sneezing and more.
The Trigeminocervical Connection: Why the Neck Matters
The trigeminal nerve doesn’t operate in isolation. In the brainstem, it converges with upper cervical spinal nerves (C1–C3) in a region called the trigeminocervical complex (TCC).
When sensory input from the face, sinuses, jaw, and neck all synapse in the same brainstem region, the brain can misinterpret the source of pain or pressure.
Neck dysfunction can present as:
“Sinus pressure”
Facial pain
Ear fullness
Headache or migraine
Sinus or facial symptoms can worsen with:
Neck tension
Poor posture
Cervical muscle spasm
Whiplash or chronic strain
Brainstem Integration: Where Trigeminal Meets Vagus
The brainstem is where they all meet. In this area:
The trigeminal nerve carries sensation from the face and sinuses
The spinal cervical nerves bring sensory information from the head, neck, shoulders, and upper limbs
The vagus nerve helps regulate heart rate, digestion, airway tone, and inflammation
Other brainstem centers integrate pain, stress, and emotional responses
Because these pathways sit so close together, sensory input from the face and sinuses can directly influence autonomic (vagal) function and vice versa.
When the vagus nerve is out of balance, it can lower the threshold for trigeminal activation, making the face, sinuses, ears, and throat more sensitive.
This helps explain why:
Stress can worsen sinus pressure
Autonomic dysfunction can cause ENT symptoms
Migraine, reflux-like symptoms, throat tightness, and dizziness often cluster together
In other words, it’s not just a sinus or throat issue-it’s a shared nervous system circuit.
So what can you do about it?
These strategies target both trigeminal nerve sensitization and vagal regulation—helping symptoms like sinus pressure, headache, throat tightness, tinnitus, and dizziness.
1️⃣ Alternate Nostril Breathing (ANB)
Why it works:
Alternate nostril breathing has been shown to balance autonomic activity by increasing parasympathetic (vagal) tone and reducing sympathetic dominance—supporting calm, balanced neural signaling. (PMID 39950247)
How to do it (3–5 minutes):
Sit comfortably with a tall spine.
Close your right nostril with your thumb, inhale slowly through the left nostril for ~4 seconds.
Close the left nostril with your ring finger, release the right, and exhale through the right nostril for ~4 seconds.
Inhale through the right, switch, exhale through the left.
Repeat for 6–10 cycles.
Why this matters:
This helps both the vagus nerve and central sensory networks settle into a regulated rhythm, lowering baseline sensitivity to facial and sinus signals.
2️⃣ Stabilize Sleep + Wake Time
Why it works:
Irregular sleep destabilizes autonomic regulation and lowers sensory thresholds, making trigeminal pathways more reactive. (PMID 36090858)
Action steps:
Same wake time daily (±30 min)
Dim lights + reduce screens before bed
Morning bright light exposure
3️⃣ Reduce Cervical & Jaw Input
Why it works (with an important nuance):
There is ongoing debate about whether neck pain triggers migraine or is actually a symptom of migraine itself. Current evidence suggests it can be both—neck and jaw tension may reflect migraine-related brainstem sensitization, while also feeding back into the trigeminocervical complex, amplifying facial, sinus, and head symptoms. (PMID 38529031)
Strategies:
Gentle cervical mobility (avoid aggressive stretching or forceful manipulation)
Heat to the neck and upper shoulders (10–15 minutes)
Jaw awareness: tongue resting on the palate, teeth unclenched
Posture support (reduce prolonged forward-head positioning)
4️⃣ Eat & Hydrate to Prevent Dips
Why it works:
Blood sugar swings and dehydration are common triggers of both trigeminal hypersensitivity and autonomic instability. In fact, new research suggests that migraine may be the result of impaired brain glucose metabolism. (PMID: 35296423)
Action steps:
Regular meals, don’t skip breakfast
Balanced macronutrients with lean protein like fish or chicken, healthy fats like olive oil and avocado, complex carbs like brown rice, potatoes and beans; replace micronutrients (most patients with migraine benefit from magnesium and vitamin B2 supplements)
Consistent fluid intake
Electrolytes if needed
5️⃣ Reduce Sensory Overload (Strategic, Not Avoidant)
Why it works:
Light, sound, screen time, and cognitive overload keep the trigeminal system in a hyper-alert state.
Action step:
Take intentional sensory breaks (quiet, dim, low stimulation)
Limit scrolling when symptomatic
Use warm light in the evening
Protect recovery time after busy days
👉 The goal isn’t avoidance—it’s lowering the background noise so the nervous system can reset.
🧠 The Big Picture
You’re not trying to “turn off” the nervous system —
you’re raising its threshold so everyday sensations don’t trigger pain, pressure, or discomfort.
Small, consistent inputs → meaningful neurologic adaptation.